Crosby Health
About Crosby Health
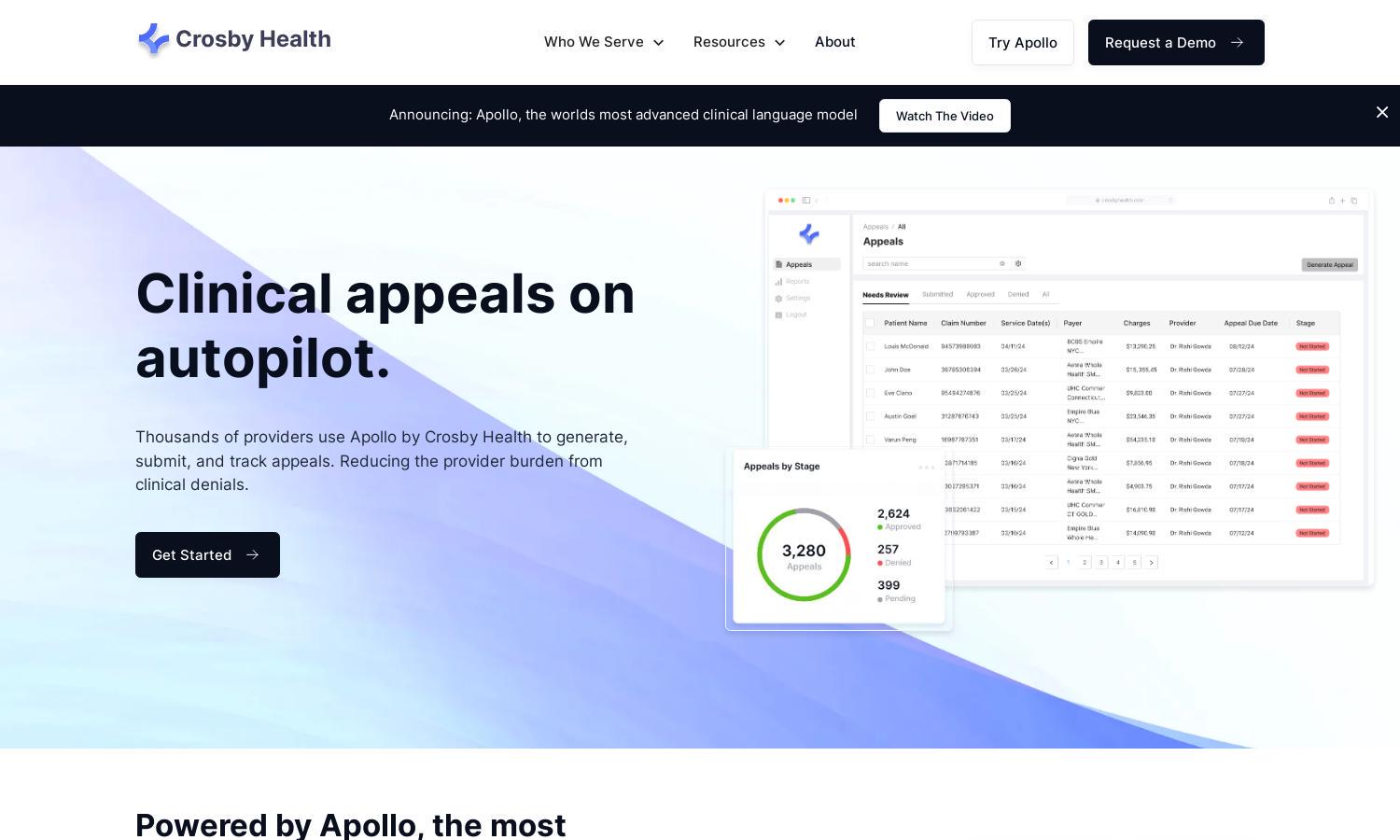
Crosby Health revolutionizes clinical appeals for healthcare entities through its advanced AI platform, Apollo. Designed for hospitals and revenue cycle management providers, it simplifies the appeal submission and tracking process. With unmatched efficiency, Crosby Health significantly reduces administrative burdens associated with clinical denials.
Crosby Health offers flexible pricing plans tailored to various business needs. Each tier provides access to essential features for automated clinical appeals, streamlining the process. Users benefit from enhanced recovery rates and reduced workloads, making upgrades appealing for maximizing financial efficiencies.
Crosby Health's user interface is crafted for ease of navigation, featuring a clean layout and intuitive design. Users enjoy a seamless experience while generating, submitting, and tracking clinical appeals. The platform's user-friendly features enhance productivity and simplify complex tasks in healthcare administration.
How Crosby Health works
Users of Crosby Health begin their journey with straightforward onboarding, where they configure their profiles and needs. The platform utilizes Apollo's advanced AI to help users generate appeal letters quickly. They can submit appeals with one-click functionality to multiple payors, all while receiving real-time updates on the status, ensuring efficient management of clinical denials.
Key Features for Crosby Health
Automated Appeal Generation
Crosby Health's automated appeal generation is a standout feature, utilizing Apollo's advanced AI technology. This function streamlines the creation of appeal letters, ensuring meticulous arguments that maximize recovery for healthcare providers facing clinical denials, ultimately saving time and effort.
Integrated Submission Process
The integrated submission process of Crosby Health simplifies how users manage appeals. This key feature allows for unified submissions to all payors via a single platform, eliminating multiple portals and enhancing efficiency, ensuring a smoother workflow for healthcare providers navigating clinical denials.
Real-Time Tracking and Notifications
Crosby Health's real-time tracking and notifications feature empowers users with immediate updates regarding appeal statuses. This capability provides enhanced visibility and control over the appeal process, allowing healthcare providers to stay informed and responsive, optimizing their management of clinical denials.
You may also like: